Upper and lower back pain can happen to anyone. Sitting in an uncomfortable chair through a long meeting can cause back pain. Even wearing the wrong type of footwear can leave your back sore and aching.
However, if your back pain suddenly appears after an accident, you may be dealing with a herniated disc, and this typically means a trip to the doctor for an exam. Thankfully, diagnosing and treating herniated discs is pretty straightforward.
If you’re not sure what a herniated disc is, what causes the issues, or even what symptoms to watch for, we’ll cover this and more in the following paragraphs.
What is a Herniated Disc
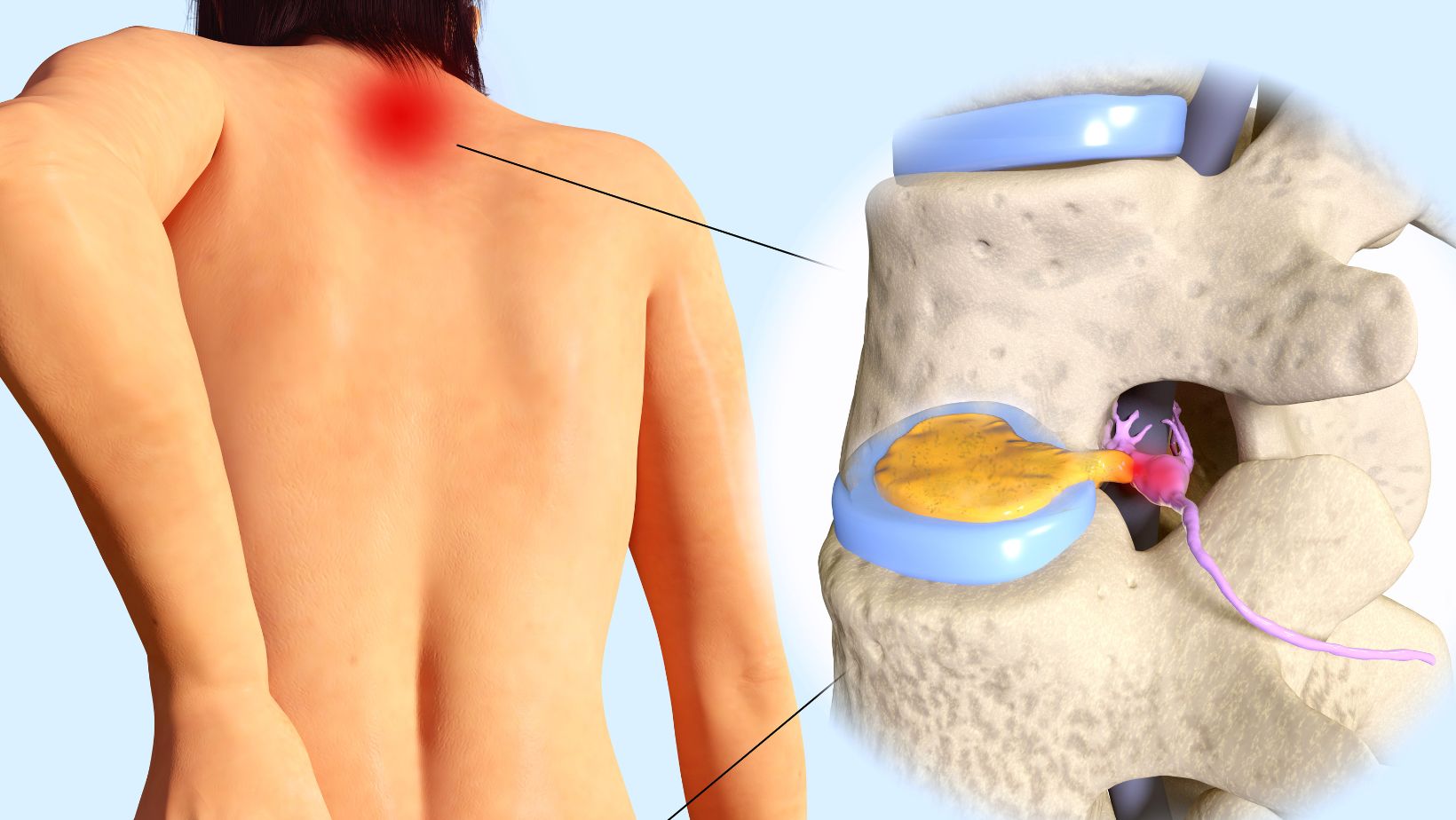
You probably already know your spine is comprised of bones known as vertebrae. In between the vertebrae are round discs that serve a vital purpose. The discs act as cushions that absorb shock. Just imagine the aches and pains you’d feel if the bones in your spinal column were constantly bumping against each other.
When a disc starts to herniated, it typically means it’s starting to degrade. The center of the disc is beginning to poke out of its hard outer shell. Since the disc takes up all of the available space between the vertebrae, even a small piece poking out can make things extremely crowded.
When this happens, part of the disc is usually pressing against a nerve. Yes, nerves are running through your spinal column, and you don’t want anything pinching or pressing down on them. While you can develop a herniated disc anywhere along your spine, most occur towards your lower back or close to the neck.
Common Causes of Herniated Discs
Unfortunately, simply getting older can cause a herniated disc, and this means that even if you’re not physically active you can still develop a herniated disc.
Think of it as part of the aging process; the discs cushioning your vertebrae can gradually degrade over time. This usually happens as the ligaments holding the discs in place start weakening. Your discs can begin to slip and end up pressing against the nerves in your spine.
Sometimes, a jarring motion can rupture a disc. For example, a hard hit is playing flag football or the force you sustain in a car accident. Twisting the wrong way, you know, trying to perform the latest dance movement, can also cause the disc to separate from your spine.
Did you know you may also be genetically prone to having disc problems? While research is still ongoing, studies suggest some individuals may be at a higher risk of developing herniated discs. If your family has a history of slipped and ruptured discs, you may have a greater chance of developing the problem.
How Do You Know if Your Disc is Herniated
Some people may not realize they have a herniated disc until they go in for an annual physical exam. Not everyone experiences back pain or even feels a slight twinge when a disc is out of place. Others may only experience a slight pain in the lower back that’s easily discounted as a normal ache, especially if it comes and goes.
Others may feel acute and intense back pain, which usually occurs when the disc is resting on a nerve. When a herniated disc is causing severe discomfort, it’s typically felt in either the lower back or around the neck.
If the pain is in the lower back, the herniated disc may be pressing against your sciatica nerve. Pain in the neck typically means the herniated disc is in the cervical spine. If you feel numbness or pain in your neck, between the shoulder blades, and even in your fingers, it’s time to contact a physician.
Diagnosing a Herniated Disc
Diagnosing a herniated disc typically starts by describing your symptoms. If you’re experiencing any pain and/or numbness in your legs, hands, and feet, make sure you let your physician know. This can help your healthcare provider narrow down the location of your herniated disc before pulling out the X-ray and other imaging equipment.
Yes, diagnosing a herniated disc means going through testing. What type of diagnostic test your physician uses depends on where you believe the herniated disc is located, along with what’s available at the clinic.
Along with taking X-rays, you may also go through a CAT scan or magnetic imaging. An electromyogram and nerve conduction study are other diagnostic options. These tests check for any potential nerve damage the herniated disc may cause. Remember, if the disc is resting on a nerve, it may be causing additional damage.
Potential Treatment Options
Being diagnosed with a herniated disc doesn’t necessarily mean an automatic appointment with a surgeon, as some herniated discs can be treated without surgery.
If you’re only experiencing mild pain without any noticeable numbness, your physician may prescribe a nonsteroidal anti-inflammatory treatment. You may also need to sit through an epidural containing a steroid. The medication is injected into your spine, close to the location of the herniated disc.
If surgery is required, the location of the herniated disc typically determines the type of procedure. You may undergo either lumbar or cervical spine surgery. Lumbar surgery treats herniated discs in the lower back. Cervical surgery deals with ruptured discs closer to the neck.
So, how do you know if you need surgery instead of a relatively non-invasive treatment like injections?
- The pain is affecting your quality of life or making it difficult to perform normal daily activities
- You’re experiencing worsening feelings of weakness and numbness in your hands or legs
- Experiencing an interruption in normal bowel and bladder functions
- Physical therapy and medication aren’t effective forms of treatment
Your physician will also examine your overall health before deciding if you’re a good candidate for herniated disc surgery.
Don’t Let a Herniated Disc Disrupt Your Life
The discs cushioning your vertebrae may be small, but when something goes wrong, the pain can be intense. Instead of letting a herniated disc disrupt your life, make an appointment with a healthcare provider. We should note that surgery may not even be necessary to correct the problem.
However, if surgery is the best treatment option, it’s worth the temporary discomfort of going through it to finally relieve your back pain.